Older adults—especially those living with chronic conditions or mobility limits—are at higher risk for urinary tract infections (UTIs). The good news: everyday caregiver actions dramatically reduce that risk. This guide distills a frontline training from Superior Health Quality Alliance into clear, do-today practices for direct caregivers in any setting and for family members caring at home.
What You’ll Learn
- Common causes and risk factors for UTIs in older adults
- Practical prevention strategies (hand hygiene, incontinence care, toileting support, catheter care, hydration)
- A quick daily checklist you can use with every shift
Why UTIs Happen: Key Risk Factors
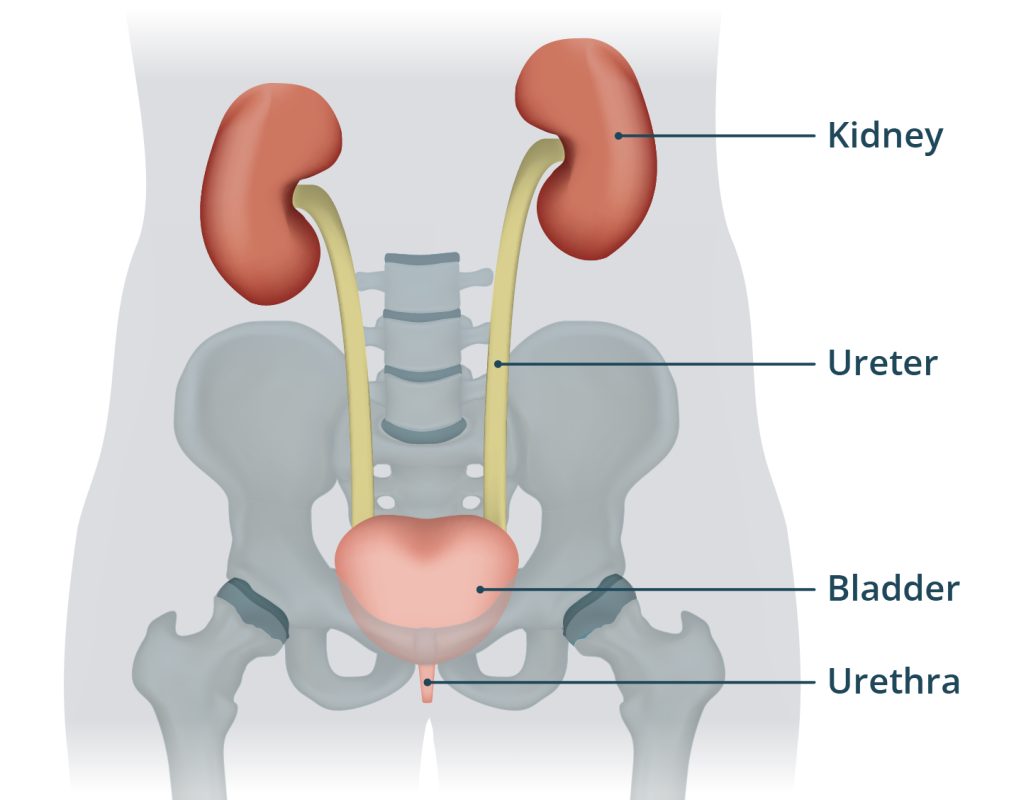
UTIs are usually caused by bacteria entering the urethra. In seniors, these factors raise the risk:
- Chronic diseases: Diabetes, heart disease, kidney disease weaken the body’s ability to fight infection.
- Neurologic conditions: Alzheimer’s, Parkinson’s, and cerebrovascular disease can cause neurogenic bladder, disrupting nerves and muscles that control urination.
- Incontinence & hygiene challenges: Fecal contamination is a major source of infection. E. coli—a normal gut bacterium—causes ~85% of UTIs. The risk rises with soiled or ill-fitting incontinence products, or when they aren’t changed often enough.
- Functional impairment: Decreased mobility makes incomplete bladder emptying more likely after voiding.
- Invasive devices: Urinary catheters provide a direct path for germs; kinks in tubing impede flow and increase risk.
- Dehydration: Infrequent drinking/urination lets bacteria build up in the urinary tract.
The #1 Prevention Habit: Hand Hygiene
Healthcare workers, on average, clean hands less than half as often as recommended. For common germs—including E. coli—alcohol-based hand rubs are more effective than plain or antimicrobial soap for hand disinfection.
Follow CDC’s “When to Clean Hands”:
- Before touching a patient
- Before an aseptic task (e.g., placing or handling devices)
- Before moving from a dirty body site to a clean site on the same patient
- After touching a patient or their immediate environment
- After contact with blood, body fluids, or contaminated surfaces
- Immediately after removing gloves
Incontinence Care That Prevents UTIs
Aim to prevent fecal soiling and support regular emptying of the bladder.
Routine Toileting
- Offer regular opportunities for toileting (scheduled rounds).
- Check for soiling frequently.
- Encourage and assist with complete bladder emptying.
Perineal Care: Step by Step
- Wash and dry your hands
- Put on gloves
- Explain what you’ll do
- Position: gently spread the legs to reach the area
- Prepare a soft, warm washcloth
- Clean front to back
- Dry with a clean cloth
- Apply cleansing lotion when needed
- Remove gloves and dispose properly
- Wash and dry your hands again
Supporting Toileting & Mobility
For anyone with mobility or cognitive impairment, assist as needed and keep toileting predictable and frequent. Small, consistent routines reduce accidents and promote full bladder emptying.
Catheter Care: Preventing CAUTI
People with Foley catheters face a higher UTI risk. Use these essentials:
- Keep catheter and tubing free of kinks
- Always keep the collection bag below bladder level
- Never rest the bag on the floor
- Empty regularly using a separate, clean container for each patient
- Avoid splashing and prevent the drainage spigot from touching non-sterile containers
- Use standard precautions (gloves, gown as appropriate) for any manipulation of the catheter or system
- Provide routine hygiene: cleanse the urethral area during daily bathing/showering
These steps lower the chance for bacteria to enter via the catheter and help prevent infection.
Hydration: A Simple, Powerful Intervention
Insufficient fluid intake is common—and preventable.
- Serve water with every meal
- Replace water pitchers every 24 hours
- Replenish each shift and as needed
- Run structured drink rounds throughout the day
A 2021 study in nursing homes showed UTI reductions when staff focused on hydration, hygiene, and catheter management—proof that everyday practices matter.
Quick Daily Checklist (Print & Post)
- ☐ Performed hand hygiene at all required moments
- ☐ Toileting offered and completed on schedule
- ☐ Incontinence products checked/changed; skin cleaned front to back
- ☐ Catheter: no kinks; bag below bladder; emptied safely; standard precautions used
- ☐ Hydration: water offered/refreshed; documented drink rounds
- ☐ Mobility support provided to promote full bladder emptying
For Family Caregivers at Home
- Keep a toileting routine (e.g., after meals, before bed).
- Prioritize hand hygiene for anyone assisting with toileting or changing products.
- Change incontinence products promptly and clean front to back every time.
- Encourage regular drinking; keep water visible and easy to reach.
- If a catheter is in place, follow the care steps above and ask your clinician to review the need for the catheter regularly.
Bottom Line
UTI prevention is built on small, consistent actions: clean hands, smart toileting and perineal care, meticulous catheter care, and steady hydration. Direct care workers and families have the power to protect seniors—every shift, every day.
Test your knowledge: https://survey.alchemer.com/s3/6961755/Front-Line-Forces-UTI-Prevention
Disclaimer
This guide is for educational purposes only and is not a substitute for professional medical advice. Follow the care plan and instructions from licensed healthcare providers. If you suspect a UTI or have questions about catheter or incontinence care, contact a clinician right away.
- “The Climb” Hits Drohan Apartments: Scaling the Leaderboard in the Battle of the Buildings!
- DASH Diet for Seniors: A Simple Guide to Lowering Blood Pressure
- Warm Hearts in a Snowstorm: The Quincy BP Challenge Hits Tobin Tower
- Common Diabetes Symptoms in Seniors: What to Watch For
- The A1C Test: Understanding Your “Big Picture” Health