High blood pressure (hypertension) is often called a “silent” condition because you usually don’t feel it. Yet over time it can quietly increase the risk of heart attack, stroke, kidney problems, and other serious health issues. That’s why many doctors now ask patients to check their blood pressure (BP) at home and bring those readings to appointments.
Home blood pressure monitoring is simple, but how you measure matters. A rushed or incorrect reading can make your numbers look higher or lower than they really are. The patient may get unnecessary medication changes—or a serious problem might be missed.
This guide walks you through a clear, three-step process—Prepare, Position, Measure—so you, your family, or your caregiver can take more accurate readings at home and share reliable results with your health care team.
Why home blood pressure monitoring is so important
There are several reasons your doctor may ask you to check your blood pressure at home:
- White-coat effect: Some people’s blood pressure rises in clinics because they feel nervous.
- Masked hypertension: Others have normal readings in the office but higher BP at home.
- Medication adjustments: Home readings help your doctor see how well your medicines are working throughout the day.
- Early warning: Regular tracking can show rising trends before they become a crisis.
When you follow a standard method every time, your readings are more dependable—and your doctor can make safer, more informed decisions.
Step 1: Prepare your body and your environment
Before you even put on the cuff, a few small actions can significantly improve accuracy.
1. Avoid things that temporarily raise your blood pressure
For at least 30 minutes before measuring, avoid:
- Caffeine (coffee, tea, soda, energy drinks, some “pre-workout” beverages)
- Smoking or vaping
- Exercise or heavy physical activity
These can cause temporary spikes that don’t reflect your usual resting blood pressure.
2. Wait after eating
If you’ve just had a meal, wait about 30 minutes before measuring. Right after eating, blood flow shifts to your digestive system, which can affect your reading.
3. Take your blood pressure before your medications (if instructed)
If you’re on blood pressure medicines, your doctor may ask you to measure before you take your dose, especially in the morning. That gives a better picture of how well the medication is working over time.
Always follow your doctor’s specific instructions on timing. If you’re not sure, ask them when they’d like you to check your BP.
4. Empty your bladder
A full bladder can raise blood pressure slightly. Try to use the bathroom first so you’re comfortable and relaxed.
5. Choose a quiet, comfortable space
Find a calm spot where you can:
- Sit comfortably
- Keep your feet flat on the floor
- Avoid interruptions from TV, phone notifications, or other people talking
Before starting, sit quietly in position for about five minutes. This “settling” time helps your body relax and gives a truer resting blood pressure.
Step 2: Position your body and the cuff correctly
Your posture and cuff placement can make a big difference. Think of this step as “setting the stage” for an accurate reading.

1. Sit with proper posture
Use a firm chair (not a soft couch or bed) and:
- Sit up straight with your back supported by the chair.
- Keep your feet flat on the floor, not on tiptoe or dangling.
- Do not cross your legs or ankles.
- Relax your shoulders and avoid leaning forward or twisting.
This position helps keep blood flow natural and even.
2. Support your arm at heart level
The arm used for measuring (usually the left, unless your doctor says otherwise) should:
- Rest on a table or armrest so it is supported, not held up in the air.
- Be at roughly the same height as your heart.
- If the arm is hanging down low, readings may be falsely high.
- If it’s too high, readings may be falsely low.
- Stay relaxed, with the palm facing up.
You should not have to hold your arm in place with muscle effort—the table or armrest should be doing the work.
3. Place the cuff correctly on your bare arm
For an upper-arm cuff (the most commonly recommended type):
- Slide the cuff onto your bare arm—not over clothing.
- Place it above the elbow, around the middle of your upper arm.
- Make sure the cuff is snug but not painfully tight. You should be able to slip one fingertip under the edge.
- Align the cuff markings (often a line or arrow) with the artery on the inner side of your arm if the manufacturer instructs this.
The key is consistency: put the cuff in the same position every time you measure.
Step 3: Take your measurements the right way
Now you’re ready to actually measure.
1. Stay still and quiet during the reading
Once you start the monitor:
- Remain silent—no talking or chatting.
- Avoid watching TV or looking at a phone.
- Keep your body relaxed and avoid moving or shifting.
Even simple actions like talking or moving your legs can raise your numbers.
2. Take multiple readings, not just one
A single reading can sometimes be off due to stress, movement, or random variation. For a more reliable picture:
- Take two or three readings in a row.
- Space them about one minute apart.
- Stay in the same position between readings.
If your doctor has asked you to track readings over time, they may suggest:
- Measuring twice a day (for example, morning and evening)
- Doing this for seven days in a row (or another period they specify)
This creates a pattern that’s much more useful than one or two isolated numbers.
3. Record your results
After you finish:
- Write down each reading with:
- Date
- Time
- Systolic (top number)
- Diastolic (bottom number)
- Heart rate, if your device gives it
- Note anything unusual, such as:
- You felt unwell or dizzy
- You were in pain
- You had just had an argument or stressful event
You can use:
- A notebook or log sheet
- A blood pressure tracking app
- A spreadsheet
- A log provided by your doctor
Bring this record to your medical appointments or share it through your patient portal if available.
Common mistakes to avoid
Even when people measure often, they sometimes fall into habits that make their readings less accurate. Try to avoid:
- Talking during the measurement
Even casual conversation can push numbers higher. - Crossing your legs
This can slightly raise blood pressure. - Measuring over clothing
A sleeve between the cuff and your skin may interfere with the reading. - Using the wrong cuff size
A cuff that’s too small can show numbers higher than they really are. If in doubt, ask your doctor or pharmacist to check the size. - Measuring when upset or in pain
If you just had a shock, bad news, or intense pain, your numbers may be temporarily high. Note this in your log.
If you realize you’ve made one of these mistakes, it’s okay. Just correct it and repeat the measurement after a few minutes of rest.
What to do with your blood pressure readings
Share them with your health care team
Bring your home blood pressure log to your appointments or send it through your clinic’s portal. Your doctor, nurse, or other clinician may:
- Look at the average of your readings over several days.
- Compare morning vs. evening numbers.
- Adjust your medications, diet advice, or lifestyle recommendations.
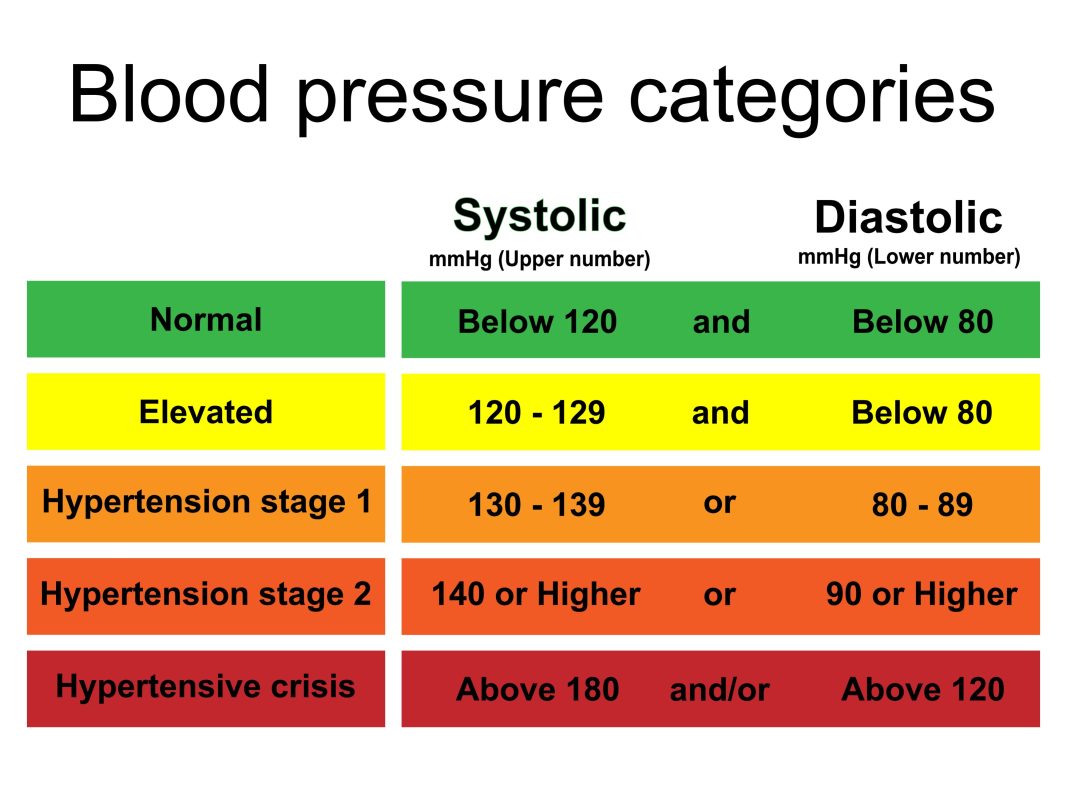
When to seek urgent help
Ask your doctor for clear guidance on when to:
- Call the office
- Call an on-call nurse line
- Go to urgent care or the emergency room
In general, if you ever have very high numbers plus serious symptoms such as chest pain, trouble breathing, sudden weakness, difficulty speaking, or vision changes—call emergency services right away. Never rely only on a blog post for urgent decisions.
Helping a loved one or senior measure blood pressure at home
Many caregivers help older adults or family members with home monitoring. A few tips:
- Explain each step calmly so the person doesn’t feel rushed or frightened.
- Make sure they are comfortable—use pillows for support if needed.
- If they have dementia or memory issues, keeping a simple routine at the same time each day can help.
- Use a written log or printed chart that you both can understand easily.
- Bring the monitor or a picture of it to medical appointments if you have questions about how to use it.
Home blood pressure monitoring can be an empowering way for patients and families to participate in care—when it’s done in a careful, consistent way.
Source
Content for this article is adapted from the “How to measure your blood pressure at home” handout, developed with permission from the American Medical Association and The Johns Hopkins University. The original copyrighted material and additional resources can be found through the AMA–Johns Hopkins blood pressure resource page.
Disclaimer
This blog post is for general information and education only. It:
- Does not provide a diagnosis
- Does not replace medical advice, examination, or treatment from a qualified health professional
- Should not be used to decide on starting, stopping, or changing any medication
Always follow the specific instructions of your doctor, nurse, or other licensed clinician. If you think you may be having a medical emergency—such as chest pain, trouble breathing, sudden weakness, confusion, or other severe symptoms—call emergency services immediately.
- “The Climb” Hits Drohan Apartments: Scaling the Leaderboard in the Battle of the Buildings!
- DASH Diet for Seniors: A Simple Guide to Lowering Blood Pressure
- Warm Hearts in a Snowstorm: The Quincy BP Challenge Hits Tobin Tower
- Common Diabetes Symptoms in Seniors: What to Watch For
- The A1C Test: Understanding Your “Big Picture” Health


