If you’re planning care for an aging parent, two acronyms keep popping up: ADLs (Activities of Daily Living) and IADLs (Instrumental Activities of Daily Living). These checklists are the backbone of senior care—they determine what help is needed, when it’s needed, and often what programs or benefits a senior can qualify for (like Adult Foster Care or in-home support). This guide breaks them down in plain language and shows how to use them to keep loved ones safe at home.
Guilding form MassHealth: [click here]
What Are ADLs?
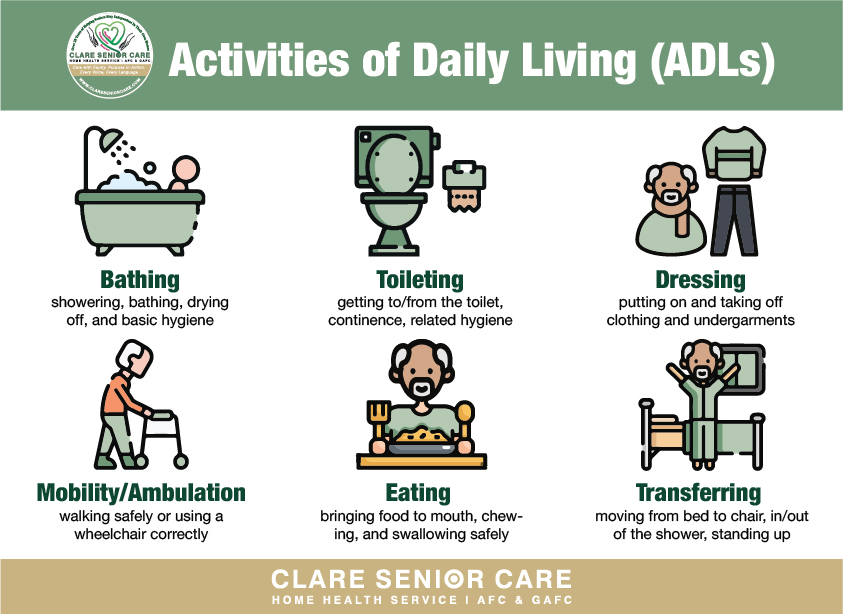
Activities of Daily Living (ADLs) are the essential hands-on tasks a person must be able to do—safely and consistently—to live independently. Most providers and insurers look at six core ADLs:
- Bathing – showering, bathing, drying off, and basic hygiene
- Dressing – putting on and taking off clothing and undergarments
- Toileting – getting to/from the toilet, continence, related hygiene
- Transferring – moving from bed to chair, in/out of the shower, standing up
- Mobility/Ambulation – walking safely or using a wheelchair correctly
- Eating – bringing food to mouth, chewing, and swallowing safely
Why ADLs matter:
- They indicate hands-on care needs and fall risk.
- They drive clinical care plans and program eligibility.
- The more help needed with ADLs, the higher the care level (and often, benefits) a senior may qualify for.
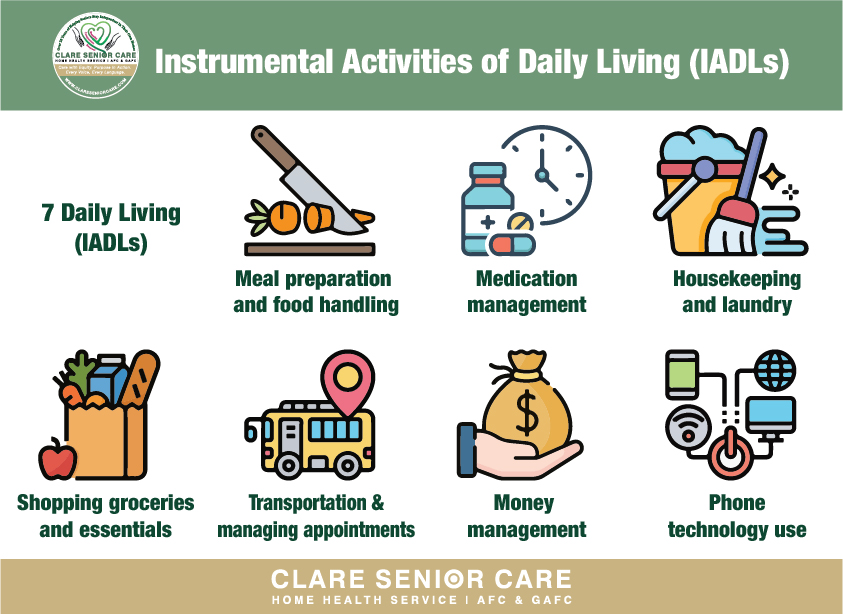
What Are IADLs?
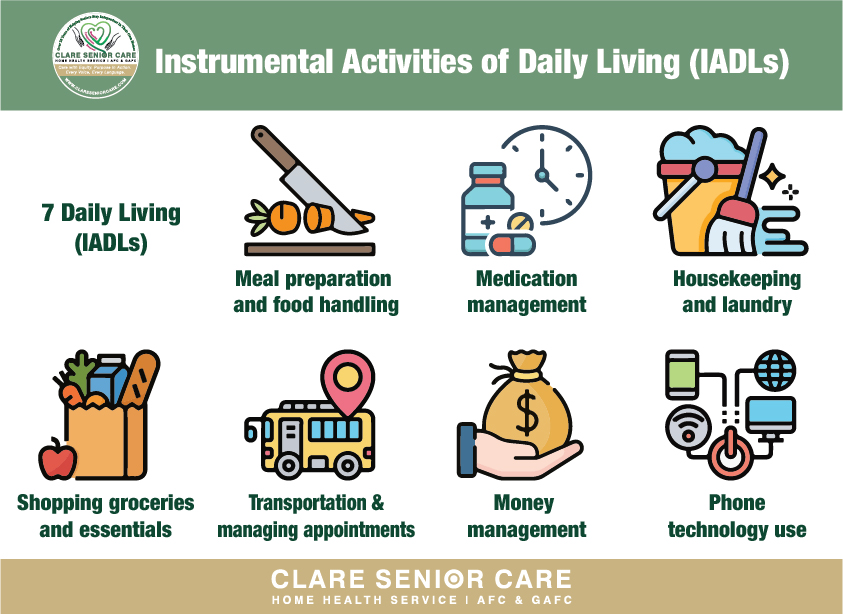
Instrumental Activities of Daily Living (IADLs) are the “life-management” tasks that keep a household running. They’re usually less hands-on than ADLs but are just as important for independence:
- Meal preparation and safe food handling
- Medication management (reminders, organizing pillboxes)
- Housekeeping and laundry
- Shopping for groceries and essentials
- Transportation/managing appointments
- Money management (paying bills, avoiding scams)
- Phone/technology use (calling for help, telehealth)
Why IADLs matter:
- They spotlight memory changes, executive function, and safety gaps (e.g., missed meds).
- They often decline earlier than ADLs—an early warning sign for families.
ADLs vs. IADLs: What’s the Difference?
- ADLs = personal, physical, hands-on tasks (e.g., bathing).
- IADLs = household, cognitive/organizational tasks (e.g., medications, money).
- Programs and insurers typically rely on ADLs to set the level of care; IADLs round out the picture and shape daily supports.
Early Warning Signs Families Should Watch
- Hygiene changes: infrequent bathing, strong odors, unchanged clothes
- Clothing/weather mismatch: winter coat in August, no coat in January
- Kitchen red flags: expired food, scorched pans, empty fridge
- Medication lapses: missed doses, double dosing
- Mobility issues: new bruises, “furniture surfing,” fear of stairs
- Paperwork piles: unpaid bills, late notices, confusion about money
- Social withdrawal: stopped calling friends or skipping appointments
These don’t mean a move to a facility. They signal it’s time to evaluate ADLs/IADLs and add supports at home.
How to Self-Check ADLs & IADLs at Home (15-Minute Method)
- List the Big Six ADLs and the IADLs that matter most for your parent.
- For each task, mark: Independent / Supervision / Partial Assist / Full Assist.
- Add notes on safety (falls, dizziness, confusion, incontinence).
- Capture medication steps (who sets up the pillbox, who reminds?).
- Identify quick wins (grab bars, pill organizer, auto-pay, rideshare schedule).
- Decide who does what (family, neighbor, paid aide, adult foster caregiver).
- Re-check every 90 days or after any hospitalization.
Pro tip: Write specific examples (“needs steadying from recliner” beats “sometimes wobbly”). Specifics translate into stronger care plans and smoother approvals for services.
Common Safety Fixes by ADL/IADL
- Bathing/Toileting: grab bars, non-slip mats, raised toilet seat, handheld shower, routine schedule
- Dressing: easy-on clothing, seated dressing, closet re-org by outfit
- Transferring/Mobility: stable shoes, cane/walker fit check, remove throw rugs, night motion lights
- Eating: adaptive utensils, small frequent meals, weekly grocery delivery
- Medications: blister packs, locked box if cognitive issues, phone/app reminders
- Housekeeping/Shopping: chore calendar, laundry day with helper, delivery services
- Money/Phone: auto-pay, spend alerts, scam awareness, large-button phone
Why ADLs/IADLs Drive Access to Services
Many supports—home health aides, Adult Foster Care (AFC), GAFC, respite, day programs—depend on documented ADL needs. In general:
- More ADL help = more hours/visits
- Higher risk (falls, wandering, forgetting meds) = stronger case
- Clear documentation (who helps, how often, what goes wrong without help) = faster approvals
If you’re in Boston, Massachusetts, a qualified agency can translate your ADL/IADL picture into a formal assessment, develop a care plan, and guide you through program eligibility.
ADLs/IADLs and Staying at Home vs. Moving
Families often ask: “Is it time for assisted living or a nursing home?” ADL/IADL findings help decide:
- Home is feasible if help covers bathing, transfers, meds, meals, and fall risks.
- Supportive housing/day programs help when IADLs are the main gaps.
- Skilled nursing/rehab may be needed if there are complex medical needs, frequent falls, or severe cognitive/behavioral risks.
The goal is not perfection—it’s a safe, sustainable plan matched to real needs.
Key Takeaways
- ADLs = hands-on personal care; IADLs = home and life management.
- They guide safety, services, and eligibility—the roadmap for staying at home.
- Specific, written examples of needs lead to faster access to the right support.
- In Boston, Massachusetts, trained teams can turn your checklist into a real care plan.
Final Thoughts
Understanding ADLs and IADLs turns guesswork into a clear plan: you’ll know what help is needed, who can provide it, and which programs can pay for it. That clarity often makes the difference between struggling alone and thriving safely at home.
👉 Ready to get started? Book a consultation or contact us to review your ADL/IADL needs and check eligibility to enroll in supportive programs that help seniors remain at home.
- “The Climb” Hits Drohan Apartments: Scaling the Leaderboard in the Battle of the Buildings!
- DASH Diet for Seniors: A Simple Guide to Lowering Blood Pressure
- Warm Hearts in a Snowstorm: The Quincy BP Challenge Hits Tobin Tower
- Common Diabetes Symptoms in Seniors: What to Watch For
- The A1C Test: Understanding Your “Big Picture” Health