Living with diabetes already means staying alert to blood sugar, medications, and daily routines. One more critical topic belongs on that list: sepsis. Sepsis is the body’s extreme, life-threatening response to an infection, and people with diabetes face a higher risk—especially from skin, foot, urinary, and lung infections. Early recognition and fast treatment save lives. Sepsis-Diabetes-2021
What is Sepsis?
Sepsis happens when an infection triggers a cascade of inflammation that can damage tissues and organs. Without rapid care, it can progress to septic shock, which is frequently fatal. Worldwide, about one-third of people who develop sepsis die, and many survivors live with long-term effects like chronic pain, fatigue, PTSD, or organ dysfunction. Sepsis is a medical emergency. If you suspect it, call emergency services immediately. Sepsis-Diabetes-2021
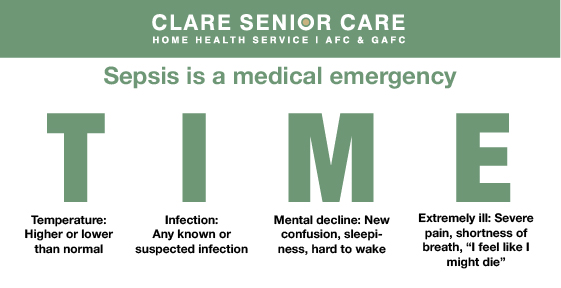
Classic Warning Signs (think T-I-M-E)
- T – Temperature: Higher or lower than normal
- I – Infection: Any known or suspected infection
- M – Mental decline: New confusion, sleepiness, hard to wake
- E – Extremely ill: Severe pain, shortness of breath, “I feel like I might die”
If these occur together, seek urgent care. Don’t wait. Sepsis-Diabetes-2021
Why Diabetes Raises Sepsis Risk
Diabetes can impair circulation and immune responses, slowing wound healing and making infections more likely and more severe. Neuropathy (reduced sensation), particularly in the feet, means cuts or blisters can go unnoticed and become infected. Any infection—skin, foot, urinary, dental, respiratory—can escalate to sepsis quickly. Sepsis-Diabetes-2021
Infection vs. Sepsis: What’s the Difference?
- Infection: Germs enter the body, multiply, and cause illness in a specific area (e.g., a foot ulcer or UTI).
- Sepsis: The body’s overwhelming and life-threatening response to that infection, leading to tissue damage, organ failure, and death if untreated.
For people with diabetes, the line from infection to sepsis can be short—act early. Sepsis-Diabetes-2021
Your Diabetes–Sepsis Prevention Plan
1) Take Care of Skin and Feet—Every Day
- Daily checks: Inspect tops, soles, and between toes. Look for redness, cracks, blisters, drainage, or warmth.
- Moisturize, but keep between toes dry.
- Trim nails carefully (or see a podiatrist).
- Protect your feet: Clean socks, well-fitting shoes; never go barefoot.
- At the first sign of a break in the skin, clean, cover, and watch closely for infection (spreading redness, swelling, pus, foul odor, fever). Seek prompt medical advice. Sepsis-Diabetes-2021
2) Prevent Infections Before They Start
- Handwashing: Do it often and well—before meals, after restroom use, and after dressing wounds.
- Vaccinations: Ask your clinician about flu and other recommended vaccines; these lower your risk of infections that can lead to sepsis.
- Dental care: Routine cleanings and quick attention to tooth or gum pain reduce hidden infection risks. Sepsis-Diabetes-2021
3) Manage Diabetes Consistently
- Keep blood glucose in target range to support healing and immune function.
- Take medications as prescribed; don’t skip insulin or oral meds.
- Address blood pressure and cholesterol, which also impact circulation and wound healing. (Good overall control reduces infection risk.) Sepsis-Diabetes-2021
4) Know When to Call the Doctor—Or 911
- Call your clinician promptly for any new wound, fever, painful urination, persistent cough, or signs of spreading skin infection.
- Call emergency services immediately if you notice T-I-M-E signs, rapid breathing, severe pain, confusion, or you simply feel “the sickest I’ve ever felt.” Sepsis-Diabetes-2021
Foot Infections: The Fast Track to Sepsis
Foot ulcers are a common infection source in diabetes:
- Small blisters or cracks can progress into deep infections.
- Poor circulation slows healing; neuropathy hides pain.
- Untreated infections can spread to the bloodstream and become sepsis.
Action steps: Daily checks, quick wound care, offloading pressure, and early medical evaluation of any concerning change. Sepsis-Diabetes-2021
Other Common Infection Sources
- Urinary tract infections (UTIs): Watch for burning, urgency, frequency, fever, back pain.
- Respiratory infections: Worsening cough, fever, shortness of breath.
- Skin/soft tissue: Redness, warmth, swelling, tenderness, drainage, or a foul smell.
- Dental infections: Toothache, swelling, fever.
Even “mild” infections can spiral—don’t delay evaluation. Sepsis-Diabetes-2021
Caregiver Quick-Check List
- Do a daily skin/foot scan (use a mirror or a helper).
- Confirm wound care supplies are on hand (saline, gauze, bandages).
- Review vaccination status.
- Reinforce handwashing habits throughout the home.
- Keep a clear plan: Who to call for new infections and which ER to use if T-I-M-E signs appear. Sepsis-Diabetes-2021
When In Doubt, Treat It Like an Emergency
Sepsis moves fast. If you’re unsure, err on the side of urgent care. Tell clinicians, “I have diabetes and I’m worried about sepsis.” Early recognition and treatment—fluids, antibiotics, and monitoring—dramatically improve outcomes. Sepsis-Diabetes-2021
Key Takeaways
- Diabetes increases the risk of serious infections and sepsis.
- Use T-I-M-E to spot sepsis early and call for help immediately.
- Daily foot/skin checks, hand hygiene, vaccinations, and good glucose control are your best prevention tools.
- Act early for any infection—small problems can become life-threatening quickly. Sepsis-Diabetes-2021
Disclaimer: This article is for education only and is not a substitute for professional medical advice. If you suspect infection or sepsis, call emergency services or go to the nearest emergency department.
- “The Climb” Hits Drohan Apartments: Scaling the Leaderboard in the Battle of the Buildings!
- DASH Diet for Seniors: A Simple Guide to Lowering Blood Pressure
- Warm Hearts in a Snowstorm: The Quincy BP Challenge Hits Tobin Tower
- Common Diabetes Symptoms in Seniors: What to Watch For
- The A1C Test: Understanding Your “Big Picture” Health